“A bit of bedlam.” That’s how the physician Graeme Clark described the scene at the Royal Victorian Eye and Ear Hospital in Melbourne, Australia, on the day before what would be the most important surgery of his career.
Engineers and staff were running around with last-minute equipment tests. Meanwhile, Clark’s patient, Rod Saunders, was relaxed. Saunders had lost his hearing in a car accident two years earlier, and Clark planned to implant a prototype device to restore at least some of Saunders’s hearing. Perhaps Saunders’s sense of calm came from the belief that his life was about to be transformed; more likely, he was feeling the effects of the Valium he’d taken.
The following day, 1 August 1978, over the course of a 9-hour operation, Clark and surgeon Brian Pyman painstakingly inserted a multichannel cochlear implant behind Saunders’s left ear. They were able to attach electrodes to the cochlea—the spiral cavity within the inner ear that stimulates the auditory nerve—without much difficulty, moving slowly and taking steps to minimize the chance of infection. The surgery appeared to be successful, but as Clark recalled in a 2011 oral history with the Australian Academy of Science, he still slept fitfully that night, worried about his patient.
Others prepared the way for Graeme Clark’s cochlear implant
Clark was not the first surgeon to implant a cochlear device, nor was Saunders the first recipient. As Albert Mudry and Mara Mills documented in their 2013 retrospective article “The Early History of the Cochlear Implant,” electrical stimulation of the ear dates to at least 1748, when Benjamin Wilson stimulated the scalp of a deaf woman with electricity. It apparently helped her hear, but Wilson couldn’t replicate the experiment on six other test subjects. In 1800 Alessandro Volta experimented on his own ear and found the entire process disagreeable and dangerous.
According to Mudry and Mills, the French physicians André Djourno and Charles Eyriès are credited as the first to insert an electrode into the auditory canal, in 1957. Theirs was not a true cochlear implant, however, nor was the cochlea mentioned in their reports. But reading an account of their operation prompted American otologist William House to begin working on a cochlear implant, in collaboration with neurosurgeon John Doyle and his brother, electronics engineer Jim Doyle.
From December 1960 to March 1961, House and the Doyles implanted devices in two patients, which they later removed. But House soon had a falling out with the Doyles, and he went on to a successful collaboration with engineer Jack Urban. Fundamental research into cochlear implants also began at other institutions. At Stanford University, otolaryngologist Blair Simmons and engineer Robert White successfully implanted the first multichannel cochlear implant, and Simmons coauthored a report about it in Science in 1965.
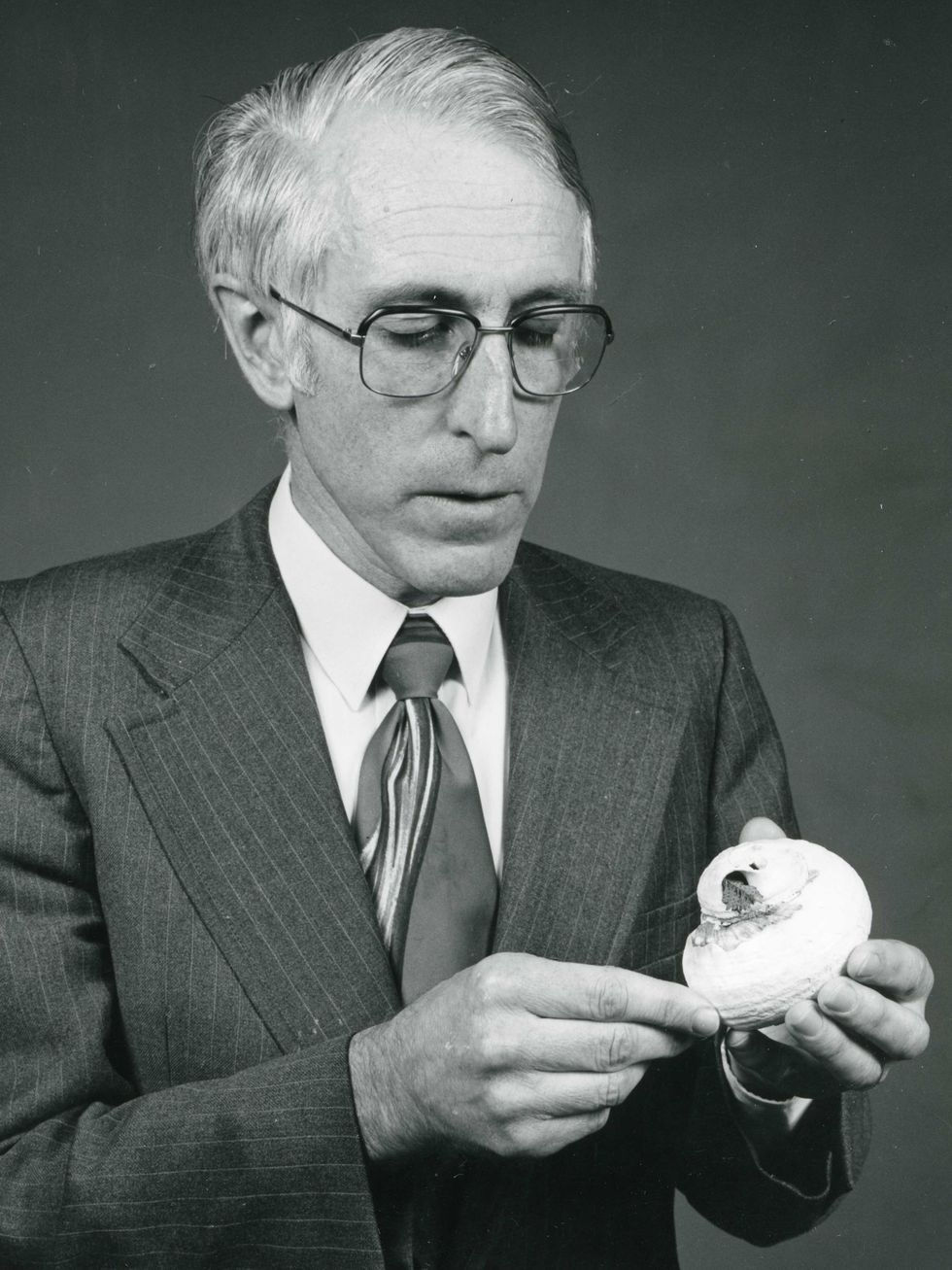
In Australia, Graeme Clark read Simmons’s report while working on his Ph.D. on neural mechanisms in hearing. Clark had trained as an ear, nose, and throat surgeon in both Australia and the United Kingdom, but he preferred research to private practice. From a young age, he understood the challenges of people who are deaf or hard of hearing because his father had poor hearing. Colin Clark was a pharmacist in the small town of Camden near Sydney. Graeme liked to play chemist in the shop and felt embarrassed whenever his father would ask customers to speak up, because everyone else in the shop would hear their business. He also saw how tiring it was for his father and how he grew isolated in social situations. At the age of 10, Graeme decided to become “an ear doctor.”
Before he succeeded, Graeme Clark faced many critics
There’s a big difference between those who have impaired hearing and those who are profoundly deaf, and research for aiding each group can diverge. The hard of hearing can still hear some sounds below 70 decibels (with varying quality depending on the level of impairment) and may be helped by hearing aids and other amplification devices.
For people who are profoundly deaf, there is an interruption of the sound signal to the auditory nerve, which can be caused by illness, trauma, or heredity. For some, like Rod Saunders, sounds of the outside world are replaced by an annoying tinnitus. Amplification will not help these individuals hear, and they rely on lipreading or sign language.
When Clark started down the path of developing cochlear implants for profoundly deaf people, he faced criticism from all directions. Leading neurophysiologists thought it was impossible to re-create hearing with electrical stimulation. ENTs argued that the surgery would be too dangerous and carry a significant risk of meningitis. Meanwhile, the legal team at the Royal Victorian Eye and Ear Hospital was concerned about liability if anything went wrong. Even his thesis director advised Clark not to pursue the topic.
Later, members of the Deaf community also criticized Clark’s work, especially when he began to experiment with cochlear implants for children. Many people who are deaf believe that being deaf is not a disability but rather a cultural identity. They saw Clark’s pediatric research as an unethical choice that parents were making on behalf of their children, depriving them of their natural culture. Operating on children under the age of four also raised concerns because it was unclear how to diagnose hearing loss accurately in children that young. Others, though, supported this type of technological intervention, and Clark’s work proceeded.
One of the key challenges was the technology itself. A basic cochlear implant consists of two parts: an external device and the actual implant. The external components include a directional microphone worn above the ear that transforms sound into a voltage waveform; a sound processor; a battery; and a transmitter that sends the wireless signal to the implant. The implant has a matching receiver that turns the signal into electric impulses and an array of electrodes embedded within the cochlea. Most of the early experiments with cochlear implants focused on single channels, or single electrodes, to excite the auditory nerve. These were cheaper and simpler to construct than multichannel implants were but had poor results when it came to speech perception. That is, patients could hear sounds but could not decipher words.
In the mid-1970s, French otolaryngologist Claude-Henri Chouard and physiologist Patrick MacLeod developed a device with seven electrodes. With each electrode placed at a different location within the cochlea, the device could operate at multiple frequencies to help produce audible sounds.
Clark was convinced that the multichannel approach was the way to go. His team included mechanical engineer Yit Chow “Joe” Tong and computer scientist J. Bruce Millar, with assistance on the electronics from Jim Patrick and Ian Forster. A major problem the team faced was how to run the wires through the spiral-shaped cochlea. In numerous interviews, Clark recalled that inspiration struck one day while he was at Minnamurra Beach watching his daughters play with a turban shell. He realized that a blade of grass with a stiff base and a flexible tip could wind through the shell, and that is how he was going to get the electrodes through the cochlea.
After years of research, and lots of experiments on cats, Clark was able to test his theories on his first human patient, Rod Saunders.
Within months, Rod Saunders comprehended speech based on electrical impulses
Despite Clark’s worries, Saunders recovered from the implant surgery without incident. Several weeks after the operation, Saunders returned to the hospital for the big test: Did the implant work? It did not. Everyone was dejected. Clark asked Saunders to come back a few days later to try again. Still no sound. Clark wondered if Saunders’s auditory nerve had been damaged in the car accident. With a damaged nerve, the implant would not work. But Clark had tested the nerve with electrical stimulation prior to the surgery and found it to have normal function.
The third time was the charm. The engineers found and fixed a loose connection in the speech processor that fitted over the implant. As they turned the electrical current up, Saunders heard a sound emerge from the background tinnitus. To test whether Saunders could sense different tones and stimulus rates, the team played “God Save the Queen.” Recognizing the tune, Saunders immediately stood to attention—a common reflex in those days for a British subject, even an Australian one—only to pull out his leads. After Saunders sat back down, the team tried out their second musical choice, “Waltzing Matilda,” and Saunders sang along.

According to Clark’s oral history, Saunders’s descriptions of the sounds helped the team refine the device. For example, the pitch of “Waltzing Matilda” was higher than Saunders could comfortably sing. He got his rhythm not from the tone, but from variations in intensity and loudness.
Over the next two months, Saunders underwent a series of psychophysical tests to determine exactly what he could hear. He also logged hundreds of hours with audiologists to fine-tune the device. In mid-December, audiologist Angela Marshall gave Saunders an open-set test, during which she could say any word in his vocabulary to determine if he could decipher speech based not on context or lipreading but on electrical stimulation alone. Saunders did not get every word, but it was enough to show that the implant was working. Clark cried tears of joy. They had proved that a cochlear implant could enable a profoundly deaf individual to hear and comprehend spoken language.
Within a year, Clark and his team implanted a device in a second patient, George Watson. Watson was a World War II veteran who had gradually lost his hearing as the result of a bomb explosion. David Dewhurst joined Ian Forster and Jim Patrick to help improve the design of the device, which Clark implanted on 13 July 1979. It worked: Watson, who had been unable to hear for 13 years, could decipher speech. This proved that the initial success was not somehow unique to Saunders’s brainwaves or condition, and it helped pave the way to commercialization of the cochlear implant.
The cochlear implant’s path to commercialization
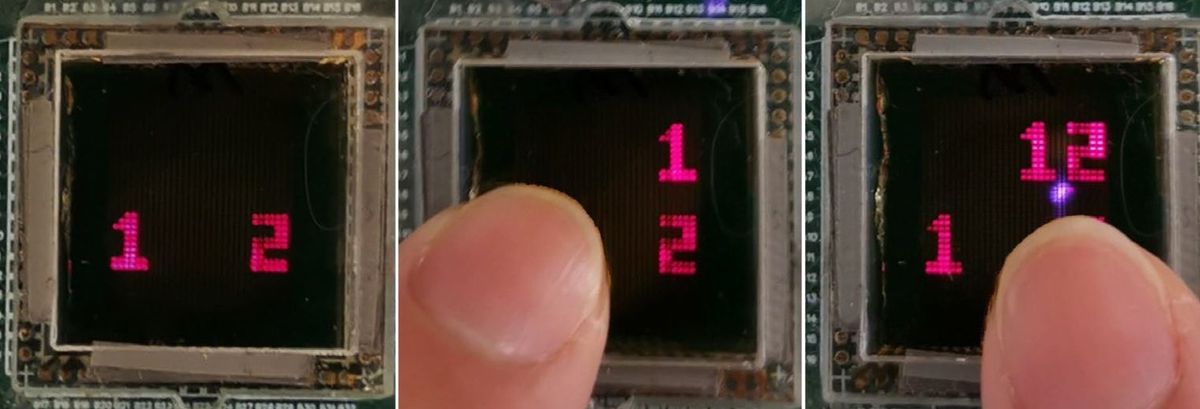
In 1979 the Australian government awarded Clark’s team a grant to further develop the implant. Even failure informed their work. In early 1980, Watson’s device stopped working, leaving him unable to hear. When the implant was removed two years later,the team discovered that electrode wires werebroken where they emerged from the device’s rigid encasement, and they determined thatsmall movementswhen Watsonchewed and rubbedhis scalp had caused metal fatigue. Clark’s team incorporated this crucial finding into a new design that was set for clinical trial. (The prototype implant pictured at top as well as the portable speech-processing unit were gifts of Graeme Clark and the University of Melbourne to the Museum of Applied Arts and Sciences in Australia.)

The first successful trial of this design took place in Melbourne in September 1982. The following year, Clark founded Cochlear Pty Ltd and joined forces with Nucleus, a medical devices company that made pacemakers, to bring the implant to market. The U.S. Food and Drug Administration approved the Nucleus cochlear implant for use in adults in 1985 and in children in 1990. Today, Cochlear Ltd is one of the leading makers of cochlear implants worldwide. In 1986, Clark established the Bionic Ear Institute (now the Bionics Institute) in Melbourne as an independent nonprofit research organization, and he served as its director until 2005.
A seashell, a blade of grass, a child’s recognition of his father’s struggles. Harsh criticism, setbacks, and decades of hard work. Graeme Clark’s journey has all the literary flourishes a novelist might look for when crafting a good tale. The fact that it actually happened is what makes my work as a historian so deeply satisfying.
Part of a continuing serieslooking at photographs of historical artifacts that embrace the boundless potential of technology.
An abridged version of this article appears in the February 2022 print issue as “Electric Hearing.”
- Middle Ear MEMS Microphone Could Restore Hearing - IEEE ... ›
- Device Uses Flashes of Light to Restore Hearing - IEEE Spectrum ›
- Optical Cochlear Implant Turns Light Against Hearing Loss - IEEE ... ›
- Restoring Hearing With Beams of Light - IEEE Spectrum ›
Allison Marsh is a professor at the University of South Carolina and codirector of the university's Ann Johnson Institute for Science, Technology & Society. She combines her interests in engineering, history, and museum objects to write the Past Forward column, which tells the story of technology through historical artifacts.