A digital microscope that uses holography and deep-learning technology could detect COVID-19 in a drop of blood. A diagnosis could be made on the spot in a matter of minutes instead of the hours or sometimes days it can take for PCR test results to come back.
The system, which uses digital holographic microscopy, could be used in areas that lack health care facilities, as well as in hospitals whose labs are backlogged with tests.
That's according to one of the machine's developers, IEEE Fellow Bahram Javidi. He is the director of the Multidimensional Optical Sensing and Imaging Systems Lab at the University of Connecticut in Storrs. His collaborators were Dr. Bruce T. Liang,Timothy O'Connor and Dr. Jian-Bing Shen. Liang is dean of the university's school of medicine, O'Connor is a biomedical engineering grad student, and Shen is a physician at the university's medical center. The researchers' article on their preliminary findings, "Digital Holographic Deep Learning of Red Blood Cells for Field-Portable, Rapid COVID-19 Screening," was published in the 15 May issue of the Optical Society's Optics Letters.
Javidi told The Institute the project stemmed from his desire to help stop the spread of the coronavirus in parts of Africa, Asia, and elsewhere that have limited resources.
"I wanted to find a way to quickly test for the virus from a droplet of blood using an affordable, portable, and rapid disease-identification system," he says.
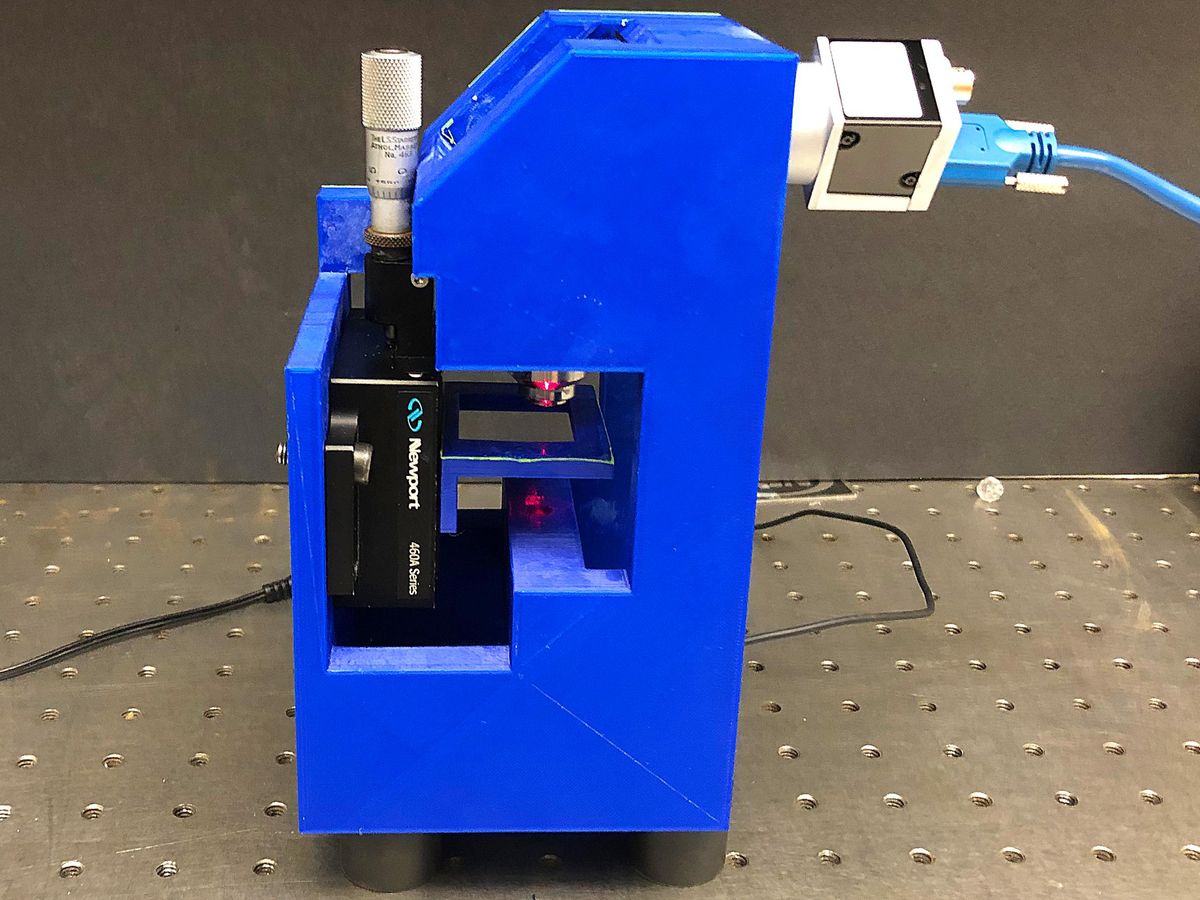
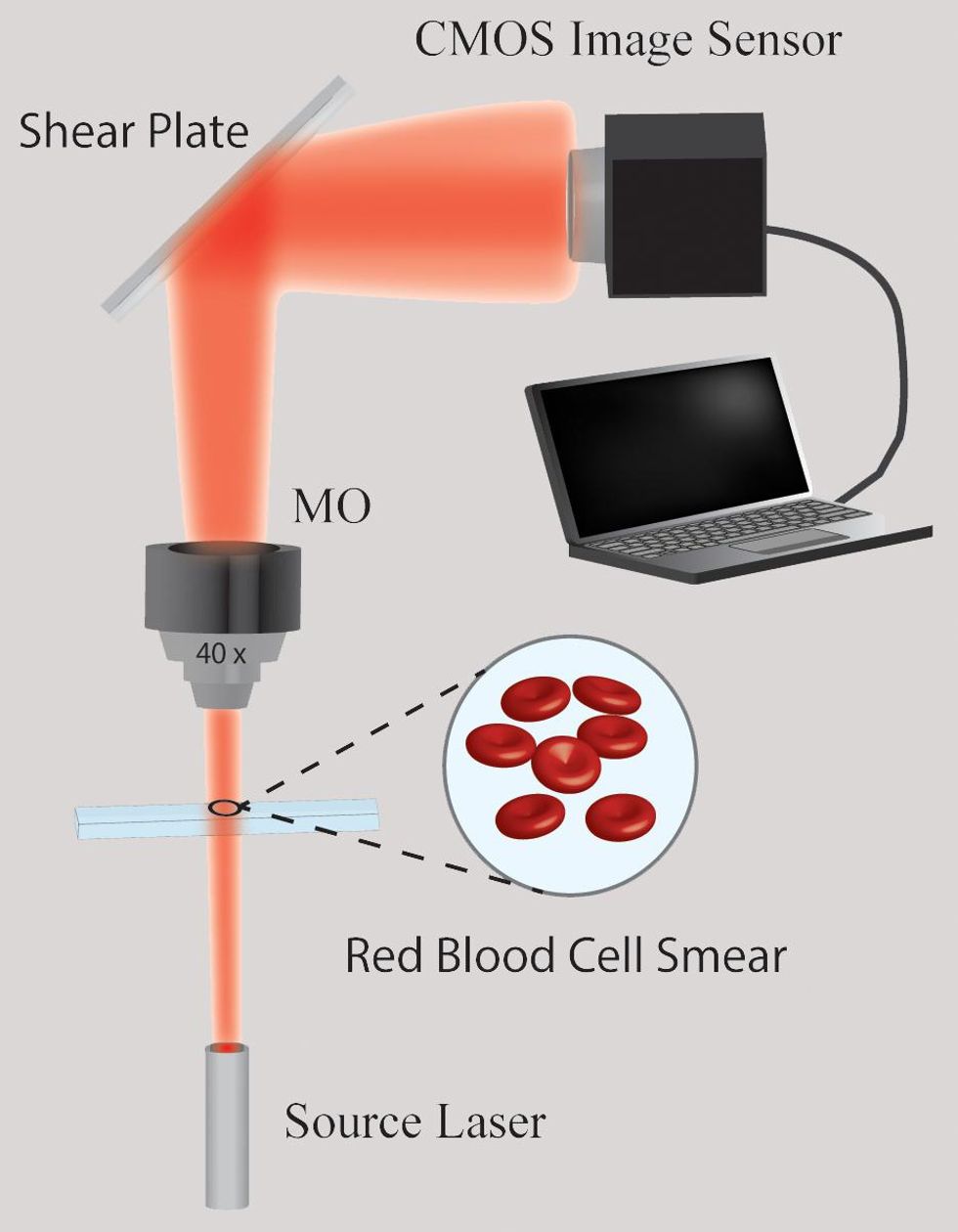
That's just what the researchers developed. The machine uses low-cost components that Javidi says can be easily obtained, including a camera, a laser diode, an objective lens, a glass plate, and a CMOS image sensor. The body of the microscope can be made using a 3-D printer.
TESTING A THEORY
A number of diseases can modify a person's red blood cells. Javidi, who is not a physician, wondered whether the same could be true of the coronavirus.
"The signatures would be very small—at the nanoscale level—but the changes in the red blood cells would still be there," he says.
He confirmed his theory with doctors at the UConn Health center. Hematologists studying COVID-19 had reported seeing changes in the blood cells of their patients, such as significantly lower hemoglobin and hematocrit levels. Furthermore, Javidi says, morphological changes have been reported in COVID-positive patients. He and his team also found recent research on COVID-19 patients that suggests statistically significant differences in the size and shape of red blood cells, especially in those with a severe case of the virus.
Javidi's research team decided to explore digital holographic microscopy, which is used in cell imaging, cell classification, and disease identification.
"DHM has drawn great interest due to its stain-free operation, numerical refocusing ability, and single-shot operation, lending itself as a powerful tool for biological sample investigation," the researchers wrote in their paper. "The technology has good vertical resolution—which helps researchers get a better sense of the morphology of cells. And because it relies on computers for much of the image processing, it is easy to use."
The technology has been able to identify malaria, diabetes, sickle-cell anemia, and other diseases through blood samples.
In the team's holographic microscope, light from the laser diode passes through the blood sample and is then magnified by an objective lens. Part of the light then bounces off the front of a glass plate and part off the back, creating two copies of the light that have passed through the sample. That creates a hologram that is then recorded by an image sensor. A technician is able to computationally work with the hologram to reconstruct a 3D profile of the sample.
"I wanted to find a way to quickly test for the virus from a droplet of blood using an affordable, portable, and rapid disease-identification system."
Individual cells are numerically reconstructed to retrieve the cells' phase profile due to the propagation and interaction of light through the cells, and then inputted into the deep-learning network to be classified.
Because no one feature of the cells was indicative of infection, the team measured a number of different features and fed them into the network to be classified.
Javidi's team worked with doctors at the university's health center to obtain the blood samples. The study looked at more than 1,400 red blood cells, with 840 of them coming from 10 patients who tested positive for the virus and 630 from 14 health care workers who tested negative. The microscope system found that 80 percent of the patients had the virus and that 13 of the 14 workers were virus-free.
The preliminary results were positive, but there were limitations to the research, Javidi says. It's not clear how effective the test will be for early detection, because the samples were taken from patients who had a moderate case of the virus.
Javidi says the next step is to continue to test blood samples of COVID-19 patients. He would like to widen the sample pool to include people outside the United States and is looking for collaborators.
He's seeking funding from the U.S. National Science Foundation.
You can learn more about the project from the lab'swebsite or by viewing this video.
Kathy Pretz is editor in chief for The Institute, which covers all aspects of IEEE, its members, and the technology they're involved in. She has a bachelor's degree in applied communication from Rider University, in Lawrenceville, N.J., and holds a master's degree in corporate and public communication from Monmouth University, in West Long Branch, N.J.